Immune Thrombocytopenic Purpura (ITP), can be defined as that disease, which results from a low number of platelets in the blood, and which hinders the clotting process. When it occurs in children, it often presents unique challenges for parents and caregivers. This article provides an in-depth look at ITP in children, including symptoms, diagnosis, treatment options, and strategies for managing the condition.
What is ITP in Children?
ITP stands for Immune Thrombocytopenic Purpura – this is a condition associated with the body’s immune system, which targets and kills platelets – cells which are believed to be responsible for blood clotting. In children ITP is usually self-limiting and may develop post viral infection. The condition can be alarming, but many children recover fully, especially with proper management and care.
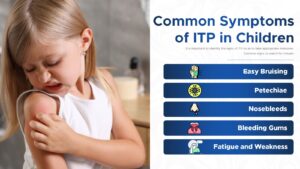
Common Symptoms of ITP in Children
It is important to identify the signs of ITP so as to take appropriate measures. Common signs to watch for include:
Easy Bruising: In cases of ITP children even get small cuts or bruises from mere bumping into something.
Petechiae: those are small round in shape, red or purple in color and they usually occur in the ankle and leg areas mostly.
Nosebleeds: Frequent or spontaneous nosebleeds can be a sign of low platelet counts.
Bleeding Gums: Unusual or excessive bleeding from the gums, especially after brushing teeth or minor injuries.
Fatigue and Weakness: There are some other symptoms that may be present but are not as common; Some children may be tired or weak.
If you observe the above signs, you should undergo an assessment with a healthcare professional.
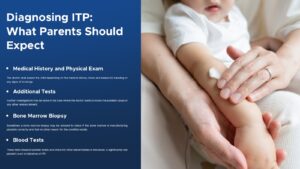
Diagnosing ITP: What Parents Should Expect
Diagnosing ITP involves several steps, and understanding the process can help alleviate concerns:
Medical History and Physical Exam: The doctor shall assess the child depending on the medical history check and assess for bleeding or any signs of bruisings.
Blood Tests: These tests measure platelet levels and check for other abnormalities in the blood. A significantly low platelet count is indicative of ITP.
Bone Marrow Biopsy: Sometimes a bone marrow biopsy may be advised to check if the bone marrow is manufacturing platelets correctly and that no other reason for the condition exists.
Additional Tests: Further investigations may be done in the case where the doctor wants to know the possible cause or any other related ailment.
Treatment Options for ITP in Children
Observation: Many children, especially those with acute ITP, may be advised to let their condition ‘watch and wait. ’ There is also a need for routine periodic checks of the platelet count.
Medications: Corticosteroids like prednisone can help increase platelet counts by suppressing the immune system’s attack on platelets. Intravenous immunoglobulin (IVIG) might also be used for short-term platelet count boosts.
Splenectomy: In chronic cases where other treatments fail, removing the spleen might be considered. The spleen is responsible for destroying platelets, so its removal can help increase platelet levels.
- Ayurvedic Herbs: Herbs like Amalaki (Amla), Known for its high vitamin C content and ability to support the immune system.Try our Amalaki Capsules. Maintaining health and enhancing your immunity is easy and accessible with Amalaki.
- Ashwagandha Often used to support overall health and vitality. We offer pure, unique formulation and in-house manufacturing to keep its effectiveness intact. Our Ashwagandha capsules contain 500 mg standardized extract of high potency.
Strategies for Children with ITP at Home
Managing ITP at home involves several strategies to help keep the child safe and healthy:
Avoiding Injuries: Encourage activities that minimize the risk of injury. For example, avoid contact sports and ensure a safe environment at home.
Monitoring Symptoms: Keep an eye on any changes in symptoms and report them to the healthcare provider. Regular check-ups will be necessary to monitor platelet levels.
Medication Adherence: In case of prescribed medications, the patients should ensure that they administer the same as prescribed and for the right dosage at the right time.
Education: Educate the child about their condition in an age-appropriate way. Understanding ITP can help them take precautions and communicate their needs.
Dietary Considerations for Children with ITP
- Pitta-Pacifying Foods: Incorporate cooling and soothing foods, such as cucumber, coconut, and mint, which help balance Pitta.
- Iron-Rich Foods: Include foods rich in iron, such as spinach and beetroot, to support blood health.
- Hydration: Promote regular intake of water to be able to maintain one’s general health and encourage essential life processes.
Coping with the Emotional Impact of ITP
The emotional impact of ITP can be significant for both the child and their family:
Emotional Support: Offer emotional support to the child so as to explain everything that he or she is going through in regard to that condition. This might include counseling or support groups for children with chronic health conditions.
Family Support: Ensure that all family members are informed and supportive. Family therapy or counseling may be beneficial if the condition causes stress or anxiety.
Encouraging Open Communication: Further, one should never shut down communication with the child and encourage them to express their emotions and report their experiences regarding ITP.
When to Seek Emergency Medical Care
Severe Bleeding: In the case of excessive bleeding or bleeding that the child cannot control, then consult an emergency doctor when the child has a cut or any kind of injury.
Signs of Internal Bleeding: Conditions such as severe or persistent belly pain, excruciating headaches non-responsive to pain killers or occurring at an unusual time of the day or night or vomiting and or passing blood should be a cause for alarm.
Sudden Changes: Any modifications regarding the symptoms or, in general, the patient’s condition, must be reported to the doctor immediately.
Long-term Outlook for Children with ITP
The long-term outlook for children with ITP varies:
Acute ITP: Most of the children live normal lives within a few months of being diagnosed with ITP with no complications.
Chronic ITP: children with chronic ITP may need further follow up but the majority can enjoy a normal, healthy and active childhood as with proper management.
Monitoring and Management: Regular follow-up with healthcare providers is essential for managing symptoms and adjusting treatment as needed.
The Role of Support Networks for Families
Care givers in the families require support networks to ensure that they help the child with the health condition as well as getting emotional support. They ease the stress by being supportive and helping with practical tasks, as well as offering essential information regarding the disease. These networks help fight isolation by connecting with other people in similar circumstances and providing help in dealing with healthcare systems. Combined, all these aspects enable families to manage the difficulties and improve their standard of living.